Author
Reviewer
Share Article
Sinking Your Teeth Into ONJ – Debunking Myths and Understanding Risks

| Author | Reviewer |
|
Aliya Khan, MD, FRCPC, FACP, FACE Professor of Clinical Medicine Divisions Endocrinology and Geriatrics McMaster University Bone Research & Education Centre Hamilton, ON |
Christine Palmay, MD, CCFP, FCFP Midtown Health and Wellness Clinic Toronto, ON |
Osteonecrosis of the Jaw (ONJ) is often a concern for patients when discussing treatments for osteoporosis.
How can we prevent it from happening? If our patients with osteoporosis want to have dental implants, does it make a difference if they're taking anti resorptive therapy for their osteoporosis? Will it have an impact on the outcome of the dental implant? These questions are valid and represent a concern for both clinicians and patients.
Let’s explore further.
Watch this video summary with blog author Dr. Aliya Khan
What is osteonecrosis of the jaw?
Simply stated, ONJ is osteonecrosis of the jaw bone in the oral cavity for eight weeks or longer in the absence of radiation therapy. Clinical examination can reveal exposed bone without a protective mucosal layer. It can be associated with pain, swelling and infection.
![]() What are the implications of osteoporosis and fractures?
What are the implications of osteoporosis and fractures?
Most cases of osteonecrosis of the jaw occur in cancer patients who are receiving high dose intravenous bisphosphonate therapy or high dose  denosumab therapy. It is also often seen in the presence of prednisone or chemotherapy.
denosumab therapy. It is also often seen in the presence of prednisone or chemotherapy.
The accumulation of exposed dead bone in the oral cavity in the absence of a local malignancy or radiation for 8 weeks or longer is consistent with a diagnosis of ONJ.
How often do we see this condition in patients with osteoporosis?
The incidence is very LOW: between 0.1 percent to less than one in a hundred thousand based on global data. Regardless, our patients are worried about osteonecrosis of the jaw if they have osteoporosis, thus representing a barrier to treatment acceptance. Furthermore, a large portion of our dental colleagues are not aware of the new global guidelines regarding diagnosis, prevention, and treatment of this condition. Perspective and context are essential.
We recently did a Canadian survey and we found that the numbers of patients with the osteonecrosis of the jaw who had osteoporosis was approximately one in a hundred thousand versus cancer patients where the numbers are much higher at approximately two per thousand.
Frankly, the incidence is very low…but the worry is high.
It’s important to remember that if a patient does develop osteonecrosis of the jaw, there could be other reasons for the ONJ and it may not have been related to the anti-resorptive therapy. Correlation does not always equate causation.
Why are we concerned about anti-resorptive therapy?
Bisphosphonates and denosumab can decrease the activity and the formation of osteoclasts. Following a dental procedure in the absence of adequate osteoclast activity, old necrotic bone may not be cleared and may accumulate in the oral cavity, in the bone, in the maxilla, or the mandible. Necrotic debris will not be removed and may become infected which can lead to osteonecrosis. An antiresorptive agent may thus impair the ability of the bone to repair and renew itself after trauma or a dental procedure in the presence of an anti-resorptive agent.
It is important to remember that it is possible that ONJ can be caused by other conditions or drugs apart from anti-resorptive therapy.
Evidence shows that a large number of other common conditions can also cause osteonecrosis of the jaw. In one study 34 of the 55 cases of ONJ were related to post surgical complications: local infections, osteomyelitis, trauma, or radiation. It doesn't necessarily have to be caused by antiosteoclast therapy.
What are the risk factors for ONJ? 
- Dental extractions
- Age – increased risk with each decade of life
- IV – Zoledronic acid infusions
- Diabetes – threefold increase
- Steroid therapy – sixfold increase
- Smoking
- Dentures especially if they are poorly fitting
- Periodontal Disease
- Poor dental hygiene
How can we minimize risk?
We all agree that optimizing oral hygiene and dental care is important as it ensures that dental caries and periodontal disease is under control. If the risk of ONJ is very high, we can reduce that risk with conservative therapy and that includes antibiotic mouth rinses and antibiotics as necessary.
 If our patient has an increased risk of ONJ and a major dental procedure is planned, then we could consider stopping anti-resorptive therapy after the surgical procedure has been completed until the surgical site heals.
If our patient has an increased risk of ONJ and a major dental procedure is planned, then we could consider stopping anti-resorptive therapy after the surgical procedure has been completed until the surgical site heals.
If they are on a bisphosphonate then they could stop the bisphosphonate, wait till everything heals up and then they could resume therapy.
If the patient is taking denosumab and the surgery that is being planned is an elective procedure, it could be scheduled to occur six months after the last denosumab dose. We would recommend waiting until the surgical site heals, which may take 4-6 weeks, and then the next dose of denosumab can be given. This would result in a delay of only 4-6 weeks for the denosumab from the due date. This would be appropriate if the risk of osteonecrosis of the jaw is high and if the risk of fracture is high. We would advise timing the oral surgery so that the denosumab is given 6 months after the last dose.
How to manage patients at high risk of fracture and also high risk of ONJ?
If the risk of fracture is high, then we could also consider teriparatide while the patient is off anti-resorptive therapy. Following healing of the surgical site then the denosumab therapy or bisphosphonate therapy can be resumed.
If the risk of osteonecrosis of the jaw is low or moderate, then we recommend stopping antiresorptive therapy if taking a bisphosphonate. If however, the patient is taking denosumab then we must recognize that cessation of denosumab is associated with a huge rise in osteoclast activity and this is associated with major increase in bone resorption. This is associated with an increased risk, in particular, of multiple vertebral fractures. Simply stated, if our patient is on denosumab, we do not want to delay that next dose of denosumab by more than four to six weeks.
What about implants?
Do anti-resorptive therapies bisphosphonates and denosumab increase the risk of dental implant failure in patients with osteoporosis? Meta-analysis showed a non-significant increased risk with anti-resorptive agents with wide confidence intervals from 0.43 to 5.70. The association between anti-resorptive therapy and dental implant failure was not confirmed.
There may be differences in bone healing after dental implant in comparison to post dental extraction. The soft tissue healing at an extraction site in comparison to what happens around a dental implant are potentially different, but we don't have sufficient data right now to provide hard concrete recommendations. 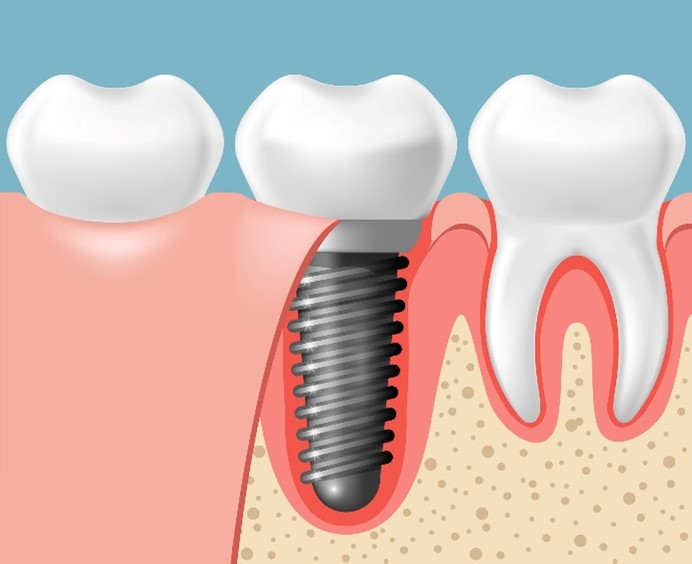 There are other comorbidities that can impact implant failure and they include diabetes, , cancer, peptic ulcer disease, glucocorticoid therapy, smoking, PPI use.
There are other comorbidities that can impact implant failure and they include diabetes, , cancer, peptic ulcer disease, glucocorticoid therapy, smoking, PPI use.
If you have osteoporosis versus, having normal bone, quantity and quality and bone strength. Is there a difference in implant failure? Will the implant not be able to remain and survive in a patient with osteoporosis, in comparison to someone who has normal bone, quality quantity and bone strength? These are valid questions and need to be proactively addressed with patients. As of today, there does not appear to be a difference in implant survival, in patients with or without osteoporosis.
![]() What about atypical fractures?
What about atypical fractures?
In summary, there is no evidence to support interruption of anti-resorptive therapy prior to implant surgery and this message must be communicated to our patients and the dental community
Do we have a consensus with our dental colleagues?
Our new guidelines are expected to be published next year! These were endorsed by the Canadian association of oral and maxillofacial surgeons, and the American association of oral and maxillofacial surgeons as well as ASBMR and the medical societies. We worked with the dentists and the oral surgeons, and there is no evidence to support stopping drug therapy prior to implant surgery. And we do know that, if we stop denosumab, it is associated with rebound increase in bone loss, and an increased risk of multiple vertebral fractures.
What about anabolic therapy?
There are no published data on the use of anabolic therapy prior to or following implant placement in patients on long-term anti-resorptive therapy.
![]() How do we identify patients at high and very high risk of fracture?
How do we identify patients at high and very high risk of fracture?
Is there an optimal time for implant placement?
Following or prior to administration of an anti-resorptive agent the risk of MRONJ may increase with surgical intervention in individuals on long-term anti-resorptive therapy. There is no evidence that stopping anti-resorptive therapy improves implant survival. It is important to remember the risk of MRONJ is low in the presence of anti-resorptive therapy in individuals with osteoporosis.
Do patients with implants require additional monitoring?
The data that we have is low quality and inconsistent, but it would be reasonable to follow these individuals.
Our evidence-based recommendations for patients with osteoporosis receiving anti-resorptive therapy suggests that anti-resorptive therapy does not need to be stopped prior to proceeding with dental implants. Of note, this a weak recommendation with very low-quality evidence and the effect of anti-resorptive therapy on implant failure is very uncertain at this time. Research is ongoing.
In conclusion anti-resorptive therapy has not been shown to increase the risk of implant failure. There's no evidence that stopping bisphosphonate or denosumab therapy improves implant survival or reduces the development of MRONJ. Cessation of denosumab is not advised as it has been associated with rebound osteoclastogenesis, and an increased risk of multiple vertebral fractures. We have all seen patients admitted to hospital with multiple vertebral fractures because they stopped denosumab prior to implant placement. It is important to emphasize that patients on anti-resorptive therapy should receive routine comprehensive oral care and regular dental examinations, and maintain good dental hygiene. These simple measures can reduce the risk of ONJ.
Continuing learning with MDLearn webcasts and podcasts:
![]() What is the impact of acute heart failure episodes on survival? - PODCAST
What is the impact of acute heart failure episodes on survival? - PODCAST
![]() How can I effectively mange my OAB patients virtually? - ACCREDITED WEBCAST
How can I effectively mange my OAB patients virtually? - ACCREDITED WEBCAST
The development of this blog was overseen by the Canadian Collaborative Research Network and was supported through an educational grant from AMGEN.
References
1. Khan AA et al JBMR 2015 Diagnosis and Management of Osteonecrosis of the Jaw: A Systematic Review and International Consensus, Khan A, Morrison A, Hanley D, Felsenberg D, McCauley L, O'Ryan F, Reid I, Rugglero S, Taguchi A, Tetradis S, Watts N, Brandi M, Peters E, Guise T, Eastell R, Cheung A, Morin S, Masri B, Cooper C, Morgan S, Obermayer-Pietsch B, Langdahl B, Al Dabagh R, Davison K, Kendler D, Sandor G, Josse R, Bhandari M, El Rabbamy M, Plerroz D, Sulimani R, Saunders D, Brown J, Compston J, J Bone Miner Res. 2015 Jan;30(1):3-23. doi: 10.1002/jbmr.2405
2. Khan AA et al JBMR 2023 – under review
copyright © 2026 CCRN
Any views expressed above are the author's own and do not necessarily reflect the views of CCRN.

